Undernutrition & Cancer: awareness to prevent

Cancer is the sixth leading cause of death in the world
With 18.1 million new cases and an estimated 9.6 million deaths in 2018 (or 1 in 6 deaths), cancer is considered by the World Health Organization (WHO) to be the sixth leading cause of death worldwide. 1 In Europe, cases represent about 1 in 5 cancer cases (23.4%) 1
Cancer patients are also malnourished!
According to the European Society for Clinical Enteral and Parenteral Nutrition (ESPEN), undernutrition is a common feature of cancer patients, regardless of the age of the patients. 2 It was shown in an Italian study in 2017 that 9% of cancer patients were undernourished at the first visit and 43% were at risk of undernutrition. 3
– On one hand, undernutrition is the consequence of both the presence of the tumor but also of medical and surgical cancer treatments. 2
– On the other hand, undernutrition also has a negative impact on quality of life and tolerance of treatment 2
ESPEN estimates that 1 to 2 in 10 cancer patients die as a result of undernutrition rather than from the tumor itself. 2
Nutrition has a special place in cancer management
There is strong evidence that nutritional issues should be addressed at the time of cancer diagnosis and should be managed in conjunction with treatment. However, cancer-related malnutrition is still largely unrecognized, underestimated, and undertreated in clinical practice. 2
How can cancer and treatment affect nutrition?
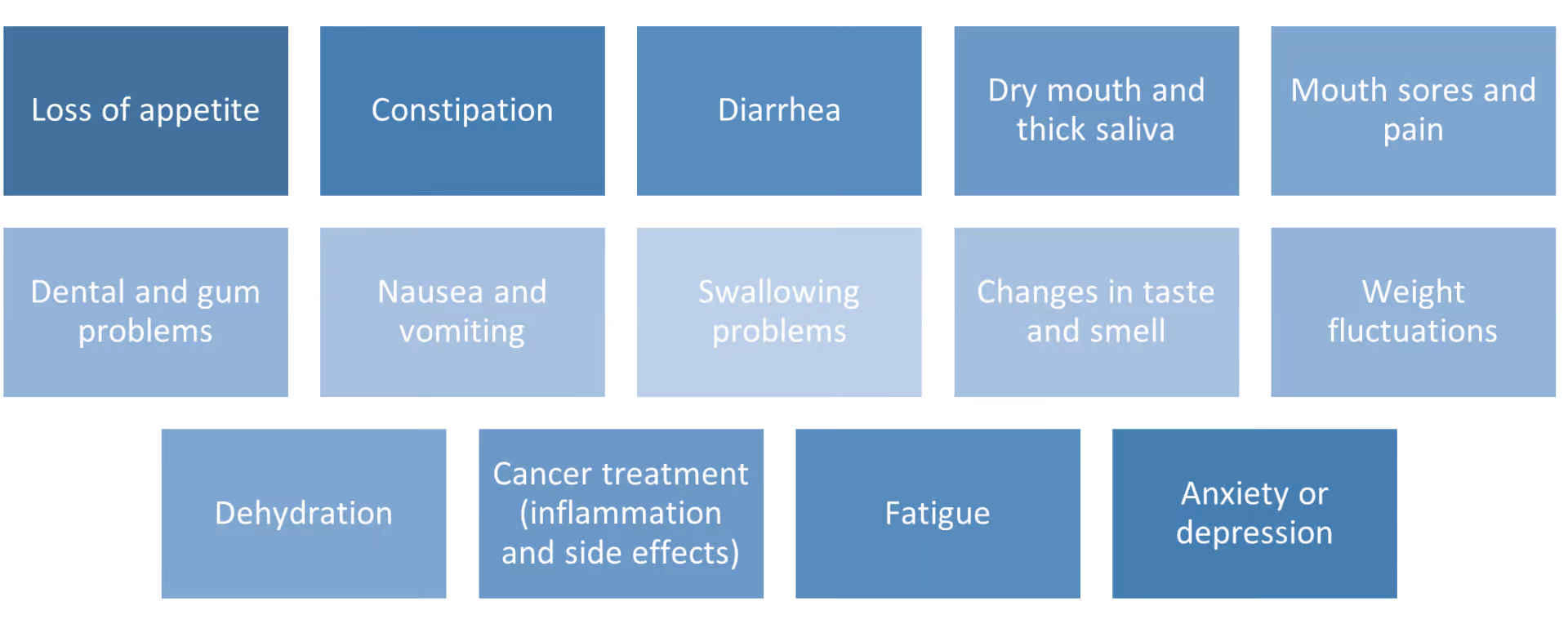
Depending on the treatment, people with cancer may experience a variety of side effects affecting the patient’s diet: 2
The diet must first and foremost meet the patient’s energy needs
As in the general population, the diet of cancer patients must absolutely meet their energy needs. This is the sum of resting energy expenditure, physical activity and, to a small extent, diet-induced thermogenesis (heat production by the body).
ESPEN assumes that total energy expenditure is the same as in a healthy individual and that the requirement is between 25 and 30 kcal/kg body weight/day. 2 This is equivalent to an intake of between 1750 and 2100 kcal for a 70 kg person.
However, studies show that about 50% of patients are hypermetabolic, i.e. have a high energy expenditure at rest.4,5 It is therefore important to provide more energy to these patients: energy requirements must be adapted.
Lipids are easily mobilized by the patient with insulin resistance compared to carbohydrates
In addition to undernutrition, cancer patients may develop metabolic disorders such as insulin resistance. In these patients, glucose uptake and oxidation by muscle cells are compromised; however, fat use is normal or even increased, suggesting an advantage for higher dietary fat intake than carbohydrate to promote efficient energy intake in these insulin-resistant patients. 2
Protein requirements are greater for cancer patients
The maintenance of muscle mass depends on the balance between the rate of muscle protein synthesis (anabolism) and breakdown (catabolism).6-8 For cancer patients, muscle protein renewal may be altered 8,9 for several reasons:
- Reduced protein intake due to anorexia related to systemic inflammation and the side effects of cancer treatment contributes to muscle loss10,11.
- In addition to reduced protein intake, muscle protein synthesis is strongly affected by physical activity levels 7,12-14, which are often decreased with cancer15-17, further exacerbating catabolism, i.e., protein breakdown.
This muscle loss among these patients is called cachexia: 50% of cancer patients are cachectic 18.
Metabolic studies have shown that a high protein intake promotes protein synthesis of muscle proteins in cancer patients19.
For this reason, the ESPEN guidelines recommend at least 1g/kg/day of protein and 1.5g/kg/day when possible 2. For example, for a person weighing 70kg, this represents between 70 and 105g of protein per day. In comparison, the European Food Safety Authority (EFSA) recommends that a healthy adult consume 0.8g/kg/day of protein.
Protein quality is just as important as quantity!
The quality of proteins is based on the measurement of its composition in essential amino acids and its digestibility. The richer a protein is in essential amino acids, the more the organism will be able to produce new proteins: this is muscle protein synthesis.
Dairy proteins, such as casein and serum proteins, are rich in essential amino acids, and therefore able to have an effect on the synthesis/degradation balance of muscle proteins. Each dairy protein has its own particularity, linked to its structure:
- In general, serum proteins, such as whey, are qualified as “fast” proteins because the passage between the stomach and the intestine is rapid and, during its digestion, the amino acids are absorbed in a short period of time20. It has been shown that the rapid arrival of amino acids in the blood, particularly leucine, could induce an increase in muscle protein synthesis21.
- Caseins are absorbed more slowly. Indeed, their coagulation in the stomach slows down their digestion, and induces a slower release in the blood, which confers to casein the capacity to both reduce the degradation of muscle proteins and also induce an increase in muscle protein synthesis. 20,22
To meet these nutritional needs, dietary advice or oral nutritional supplements are recommended.
This advice includes: 2
- In the first instance, dietary counseling to encourage the intake of energy and protein rich foods and beverages to maintain or improve nutritional status.
- Treatment of symptoms that have a direct impact on food intake, including anorexia
- Offer Oral Nutritional Supplements (ONS) when food fortification is not sufficient to achieve nutritional goals
This nutritional management is best initiated when the patient is not yet severely malnourished. 2
ONS supplementation is recommended when the fortified diet is not effective in achieving nutritional targets. Indeed, they are indicated when the patient is not able to eat more than 50% of the nutritional intake target in one week or between 50 and 75% of the requirements in 2 days. 2
Our ONS help to achieve the nutritional targets:
| Fortified drink | 1 drink provides (% of needs) |
Fortified cream | 1 cream provides (% of needs) |
|
| Energy (Kcal) | 360 to 460 | 17-26% | 300 | 14-17% |
| Protein (g) | 20-29 | 19 to 41% | 14 | 13-20 |
Conclusion
Oral clinical nutrition products help to perfectly meet the needs of undernourished and cancer patients.
For more information on our range of oral clinical nutrition products, please feel free to reach us via our contact form.
Author: Emmeline SALAMEH
Emmeline SALAMEH is a doctor in physiology and nutrition. Based in Retiers, she is a member of the Nutrition department of Lactalis Research & Development and is specialized in clinical nutrition.
REFERENCES
- Bray, F. et al. Global cancer statistics 2018: GLOBOCAN estimates of incidence and mortality worldwide for 36 cancers in 185 countries. CA. Cancer J. Clin. 68, 394–424 (2018).
- Muscaritoli, M. et al. ESPEN practical guideline: Clinical Nutrition in cancer. Clin. Nutr. Edinb. Scotl. 40, 2898–2913 (2021).
- Muscaritoli, M. et al. Prevalence of malnutrition in patients at first medical oncology visit: the PreMiO study. Oncotarget 8, 79884–79896 (2017).
- Bosaeus, I., Daneryd, P., Svanberg, E. & Lundholm, K. Dietary intake and resting energy expenditure in relation to weight loss in unselected cancer patients. Int. J. Cancer 93, 380–383 (2001).
- Cao, D. et al. Resting energy expenditure and body composition in patients with newly detected cancer. Clin. Nutr. Edinb. Scotl. 29, 72–77 (2010).
- van Vliet, S., Burd, N. A. & van Loon, L. J. The Skeletal Muscle Anabolic Response to Plant- versus Animal-Based Protein Consumption. J. Nutr. 145, 1981–1991 (2015).
- Wolfe, R. R. Regulation of Muscle Protein by Amino Acids. J. Nutr. 132, 3219S-3224S (2002).
- Phillips, S. M., Glover, E. I. & Rennie, M. J. Alterations of protein turnover underlying disuse atrophy in human skeletal muscle. J. Appl. Physiol. 107, 645–654 (2009).
- van der Meij, B. S., Deutz, N. E. P., Rodriguez, R. E. R. & Engelen, M. P. K. J. Increased amino acid turnover and myofibrillar protein breakdown in advanced cancer are associated with muscle weakness and impaired physical function. Clin. Nutr. 38, 2399–2407 (2019).
- van der Meij, B. S., Teleni, L., Engelen, M. P. K. J. & Deutz, N. E. P. Amino acid kinetics and the response to nutrition in patients with cancer. Int. J. Radiat. Biol. 95, 480–492 (2019).
- Dodson, S. et al. Muscle Wasting in Cancer Cachexia: Clinical Implications, Diagnosis, and Emerging Treatment Strategies. Annu. Rev. Med. 62, 265–79 (2011).
- Paddon-Jones, D., Short, K. R., Campbell, W. W., Volpi, E. & Wolfe, R. R. Role of dietary protein in the sarcopenia of aging. Am. J. Clin. Nutr. 87, 1562S-1566S (2008).
- Phillips, S. M. Nutrient-rich meat proteins in offsetting age-related muscle loss. Meat Sci. 92, 174–178 (2012).
- Deutz, N. E. P. et al. Muscle protein synthesis in cancer patients can be stimulated with a specially formulated medical food. Clin. Nutr. 30, 759–768 (2011).
- Hasegawa, Y. et al. Protein intake after the initiation of chemotherapy is an independent prognostic factor for overall survival in patients with unresectable pancreatic cancer: A prospective cohort study. Clin. Nutr. 40, 4792–4798 (2021).
- Lawson, C., Ferreira, V., Carli, F. & Chevalier, S. Effects of multimodal prehabilitation on muscle size, myosteatosis, and dietary intake of surgical patients with lung cancer — a randomized feasibility study. Appl. Physiol. Nutr. Metab. 46, 1407–1416 (2021).
- Smith, W. A., Nolan, V. G., Robison, L. L., Hudson, M. M. & Ness, K. K. Physical activity among cancer survivors and those with no history of cancer— a report from the National Health and Nutrition Examination Survey 2003-2006. Am. J. Transl. Res. 3, 342–350 (2011).
- Tisdale, M. J. Mechanisms of cancer cachexia. Physiol. Rev. 89, 381–410 (2009).
- Baracos, V. E. Skeletal muscle anabolism in patients with advanced cancer. Lancet Oncol. 16, 13–14 (2015).
- Boirie, Y. et al. Slow and fast dietary proteins differently modulate postprandial protein accretion. Proc. Natl. Acad. Sci. U. S. A. 94, 14930–14935 (1997).
- Jäger, R. et al. International Society of Sports Nutrition Position Stand: protein and exercise. J. Int. Soc. Sports Nutr. 14, 20 (2017).
- Devries, M. C. & Phillips, S. M. Supplemental Protein in Support of Muscle Mass and Health: Advantage Whey. J. Food Sci. 80, A8–A15 (2015).



