Minerals and vitamins in childhood: Focus on Calcium, Vitamin D and Iron

uring early days of life, ensuring growth is key. During this period, it is therefore particularly important to provide all the vitamins and minerals necessary for the development of the whole body including bones structure, organ functions but also cognitive capacities. In this article, we have chosen to focus on three of them: calcium and vitamin D for the bone building as well as iron for cognitive development.
Calcium: Building blocks of bones thanks to the help of Vitamin D
Calcium is an integral component of the skeleton; approximately 99 % of total body calcium is found in bones and teeth. Calcium has a structural role, and is needed for bone rigidity, strength and elasticity (1). Vitamin D, has two origins: from the diet and from the skin under the influence of ultraviolet B-light. The principal function of vitamin D is to maintain calcium concentrations at a sufficient level to support cellular processes, neuromuscular function and bone ossification. This regulation is accomplished by enhancing the efficiency of the intestine to absorb dietary calcium and also by mobilizing calcium from the bones (1,2). Thus, if calcium is ingested in the meantime than vitamin D: its intestinal absorption will be more efficient.
Conversely, if the dietary supply of calcium is insufficient to meet physiological requirements, calcium may be resorbed* (*taking apart) from the skeleton so the body can use it for other priority physiological functions. Early signs of vitamin D deficiency include decreased blood concentrations of calcium and might lead to rachitism later in life. Later signs of calcium and Vitamin D deficiencies comprise inadequate skeletal mineralization (rickets and osteomalacia), bone deformities, bone pain, and alterations in muscle metabolism and respiratory function (1,2).
The breastmilk as the gold standard
Calcium in breast milk is found to be in the range of 200-300 mg/L (1). Main sources of calcium in human breast milk are the liberation of calcium through increased bone resorption during lactation, upregulation of intestinal calcium absorption, and, with a lesser extent, dietary intake (3). By calculating the amount of breastmilk generally consumed in this age group, the EFSA experts stated that a 0-6 month- old infant must consume 200 mg / day.
The average vitamin D content of breast milk in healthy women has been reported to be in the range 0.25-2.0 μg/L (0.04-0.31 μg/100 kcal) (1). There is general agreement that human milk does not contain sufficient vitamin D to prevent inadequate skeletal mineralization (3,4). According to EFSA experts, a vitamin D intake of 10 μg/day is adequate for the majority of infants below 6 months having minimal sun exposure.
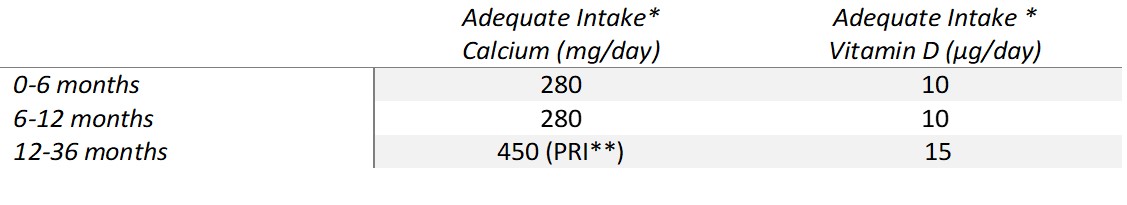
The adequate intakes as defined by EFSA for Calcium and Vitamin D for infants from 6-12 months and 12-36 months are described below.
* An adequate intake (AI) is used when there isn’t enough data to calculate an average requirement. An AI is the average nutrient level, based on observations or experiments that is assumed to be adequate for the population’s needs.
** PRI : The population reference intake (PRI) is the intake of a nutrient that is likely to meets the needs of almost all healthy people in a population.
Because bone formation is key during childhood, providing the right amounts of calcium and vitamin D through infant formula when breastfeeding is not possible is essential. (5).
Iron : key player in brain development
Growth and development of the central nervous system is rapid during the first years of life, the human brain almost triples its weight from birth to 3 years of age and has, at that age, reached 85% of its adult size. Iron is an essential trace element that has important metabolic function such as oxygen transport and is involved in many metabolic reactions. Moreover, scientific studies have shown that through these functions, iron is essential for several aspects of brain development: myelination, neurotransmitter function and neuronal energy metabolism (2,6,7).
However, Iron deficiency remains the most common micronutrient deficiency worldwide. It is a critical global health problem given the persistence of its high prevalence in many countries and also the subsequent health consequences, including brain dysfunction. In 2019, the worldwide prevalence of anemia was approximately 40% in children <5 years, reaching almost 60% in Africa (6). Young children are a special risk group because of their rapid growth that leads to high micronutrients requirements such as iron . Moreover, highly bioavailable dietary iron comes mainly from meat, the intake of which is low in children. Risk factors associated with a higher prevalence of iron deficiency include low birth weight, high cow’s-milk intake, low intake of iron-rich complementary foods, low socioeconomic status from birth to school-age (6,7).
The breastmilk as the gold standard
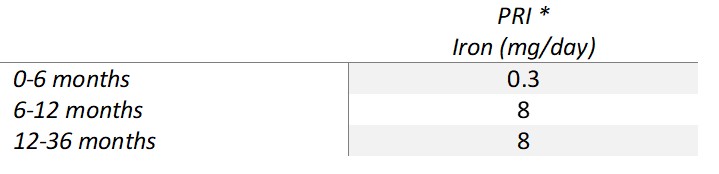
The iron concentration in human milk is around 0.2-0.4 mg/L (0.03-0.06 mg/100 kcal) (1). Full-term infants have iron stores sufficient to cover their needs for a couple of months (1). The experts from EFSA considered that a minimum intake of 0.3 mg/day are generally sufficient to ensure the iron needs in the first half-year of life for most healthy term infants in industrialized countries. When iron is provided through formula, in which it is assumed to be less available than in breast milk. Additional dietary iron needs to be provided in these formulae in order to ensure a sufficient iron supply to formula-fed infants. That’s why, EFSA experts recommend a minimum of 0.3 mg / 100 Kcal of formula, a 10 time higher amount that found in breastmilk which represent an intake of 1.5 mg of iron / day. For the second half-year of life, the experts considered an iron intake of 8 mg/day adequate for the majority of infants (1).
Specific FOCUS on 12-36 months:
Along all of the preadolescent age groups, the prevalence of iron deficiency is highest among toddlers (1-3 years old) (6). The cohort study called Nutribébé performed in France in 2013 showed that 25% of infants aged 10-23 months and more than 50% of older children (3 years old) had an iron intake lower than recommended (8). This iron deficiency has been also confirmed in others European countries (9). Thus, usual dietary recommendations suggest the primary use of iron-containing solid foods and, in formula-fed infants, the prolonged consumption of fortified young child infant formula (6,10).
*PRI : The population reference intake (PRI) is the intake of a nutrient that is likely to meets the needs of almost all healthy people in a population.
Iron is essential for all aspects of brain development but also for other biological functions, and the consequences of iron deficiency can be seen as poor immune function or impaired cognitive performances.
Mathilde Guerville is a nutrition scientist who works in the R&D Nutrition department of Lactalis. She is a dietician and completed her training with a PhD in nutrition in Rennes. She manages clinical studies on nutrition and health and participates in the development of innovative products for a number of targets including infants and the elderly.
Bibliography
- EFSA (European Food Safety Authority). Scientific Opinion on nutrient requirements and dietary intakes of infants and young children in the European Union1. EFSA JOURNAL. 2013;
- ANSES. Les références nutritionnelles en vitamines et minéraux. Avis de l’Anses Rapport d’expertise collective. Mai 2021.
- Bae YJ, Kratzsch J. Vitamin D and calcium in the human breast milk. Best Pract Res Clin Endocrinol Metab. 1 janv 2018;32(1):39‑45.
- Olafsdottir AS, Wagner KH, Thorsdottir I, Elmadfa I. Fat-soluble vitamins in the maternal diet, influence of cod liver oil supplementation and impact of the maternal diet on human milk composition. Ann Nutr Metab. 2001;45(6):265‑72.
- EFSA (European Food Safety Authority). Scientific Opinion on the essential composition of infant and follow-on formulae. EFSA J. 2014;12(7):3760.
- Chouraqui JP. Dietary Approaches to Iron Deficiency Prevention in Childhood—A Critical Public Health Issue. Nutrients. 12 avr 2022;14(8):1604.
- Domellöf M. Iron requirements, absorption and metabolism in infancy and childhood. Curr Opin Clin Nutr Metab Care. mai 2007;10(3):329‑35.
- Chouraqui JP, Tavoularis G, Turck D, Ferry C, Feillet F. Mineral and vitamin intake of infants and young children: the Nutri-Bébé 2013 survey. Eur J Nutr. sept 2020;59(6):2463‑80.
- Hojsak I, Bronsky J, Campoy C, Domellöf M, Embleton N, Fidler Mis N, et al. Young Child Formula: A Position Paper by the ESPGHAN Committee on Nutrition. J Pediatr Gastroenterol Nutr. janv 2018;66(1):177‑85.
- ANSES. Avis de l’Agence Nationale de Sécurité Sanitaire de l’Alimentation, de l’Environnement et du Travail relatif à l’actualisation des repères alimentaires du PNNS pour les enfants de 4 à 17 ans. Saisine n°2017-SA-0142; 2019.